Medicine Turns to Nature

THROUGHOUT MEDICINE, RESEARCHERS HAVE TURNED TO NATURE FOR COMPOUNDS TO PROMOTE HEALING. AT SAINT JOHN’S CANCER INSTITUTE, RESEARCHERS ARE EXPLORING THE CANCER-FIGHTING PROPERTIES OF COMMON WHITE BUTTON MUSHROOMS, AGARICUS BISPORUS, WHILE PACIFIC NEUROSCIENCE INSTITUTE SCIENTISTS ARE INVESTIGATING THE EMOTIONAL HEALING POTENTIAL OF GENUS PSILOCYBE MUSHROOMS.
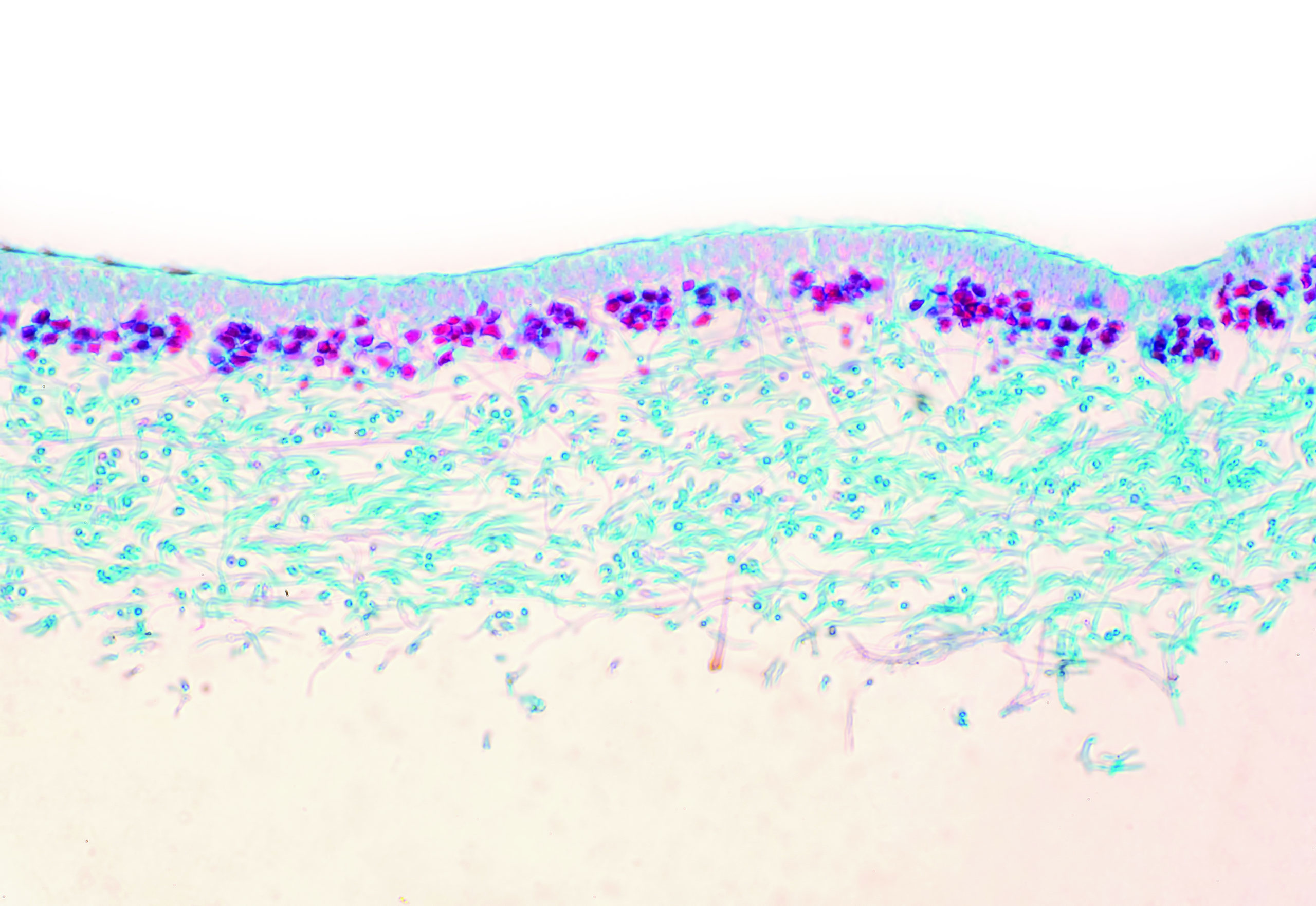
THE CANCER-FIGHTING POTENTIAL OF AGARICUS BISPORUS
Every year, about 1 in 8 men in the U.S. will be diagnosed with prostate cancer. Przemyslaw Twardowski, MD, director of clinical research, urology and urologic oncology at Saint John’s Cancer Institute, hopes to expand treatment options for these patients through two clinical trials conducted in partnership and collaboration with City of Hope. These clinical trials, funded by a National Cancer Institute RO1 Grant and based on Dr. Twardowski’s previous research, will examine the potential cancer-fighting properties of common white button mushrooms, or agaricus bisporus. Both clinical trials will be conducted over a one-year period and focus on patients with early stages of prostate cancer who will be administered tablets derived from agaricus biporus. The first group consists of patients who have had surgery or surgery with radiation and had a good postsurgical prognosis. However, later their PSA—or prostate-specific antigen, a protein produced by the prostate gland—has gone up, which suggests that the cancer is not cured. “They don’t have any visible cancer activity, like CT scans or bone scans, but their elevated PSA is a harbinger that some residual cancer is resurfacing,” says Dr. Twardowski. “With this group, we will be testing whether the mushroom treatment will stabilize or hopefully lower the PSA.” The second group of patients have been recently diagnosed with prostate cancer but have not been treated because their cancer is slow growing. “Typically, these types of patients are put on what’s called active surveillance which includes MRI-type scans, PSA monitoring and periodic biopsies to see if the cancer becomes more aggressive before treatment is instituted,” says Dr. Twardowski. “So these patients will be given the mushroom tablets to see if we can essentially prevent the need for future treatment over the length of the program.” For the first three months of the study, only half the participants in both groups will receive the treatment so the mushroom tablets’ effectiveness can be measured against the control group. However, after three months the tablets’ initial effectiveness will be evaluated, and all participants will have an opportunity to receive the treatment.
STUDYING NATURE WITH SCIENTIFIC RIGOR
As an oncologist with a subspecialty in prostate, bladder, kidney and testicular cancers, Dr. Twardowski has lectured both nationally and internationally, has been extensively published, and has been a principal investigator and contributor to hundreds of clinical trials that have advanced treatment options for patients. His research in the curative potential of white button mushrooms was inspired by his cancer patients’ interest in dietary and natural substances to improve their health as well as early research by his collaborator, Shiuan Chen, PhD, of City of Hope, into the cancer-fighting properties of agaricus bisporus. “Many patients in my practice—and I think this is the case in oncology in general—take multiple over-the-counter supplements on their own, but it’s often based on sketchy and limited scientific evidence,” he says. “Yet I do believe there may be certain types of natural products that do have legitimate anticancer effects that need to be studied in a more scientific, rigorous way.” The current trial is based on previous research he conducted in collaboration with Chen which suggested white button mushrooms had anti–prostate cancer properties. That study, published in May 2015 in the American Cancer Society journal Cancer, demonstrated that 30% of patients with relapsing prostate cancer after surgery who were treated with agaricus bisporus had decreased PSA levels. If these new clinical studies support the previous research, then further investigation will be needed to discover the actual mechanism behind agaricus bisporus’ cancer-fighting ability. Dr. Twardowski hypothesizes that it relates to cancer immunotherapy, a form of treatment that uses the body’s immune system. “In our preliminary studies, both in those based on blood samples from patients we’ve treated and laboratory work, it seems that there are certain aspects of the anticancer immune system that are accelerated by the treatment with this mushroom tablet,” he says. “Discovering this mechanism would be the next exciting step in this research.” Philanthropic funding will help power this promising research, Dr. Twardowski says, by permitting the researchers to instinctively follow nature’s signposts. “Philanthropy gives us flexibility to explore deeper levels than what may be possible with a government grant,” he says. “It is vital for moving the field of cancer research forward.”

PSILOCYBIN AND THE TRIP PROGRAM
A growing body of research now supports the potential use of mushrooms containing the chemical psilocybin for a range of cognitive, mental and behavior disorders. Several research projects at Pacific Neuroscience Institute at Providence Saint John’s Health Center are aimed at determining the safety and efficacy for psilocybin-based therapies, says Keith Heinzerling, MD, an addiction medicine specialist and well-published clinical investigator. Dr. Heinzerling recently joined Pacific Neuroscience Institute as director of its new Pacific Treatment & Research in Psychedelics (TRIP) Program. Psilocybin, which is found in a range of genus Psilocybe mushrooms, has been the subject of decades of research for treating such conditions as depression, anxiety, post-traumatic stress disorder (PTSD) and drug and alcohol use disorders. PNI researchers are launching several clinical trials to investigate the life-changing possibilities of psilocybin, Dr. Heinzerling says. “My goal for the TRIP Program is to provide very sound scientific methods, innovation and compassionate care,” says Dr. Heinzerling. TRIP researchers are currently conducting a clinical trial using psychotherapy combined with psilocybin for patients with alcohol use disorder. Other TRIP studies are in early stages, including one to help patients undergoing the complicated grief of losing a loved one to COVID-19 and another for terminal cancer patients experiencing psychological distress caused by their diagnosis. These studies all follow strict safety protocols and adhere to long-held concepts on the importance of set and setting. Consenting and eligible patients are first provided with psychotherapy sessions to prepare them to optimize their mindset. The actual psilocybin treatment or journey which lasts four to five hours takes place in a controlled setting in a comfortable room with eyeshades and music, under the supervision of two trained professional guides. In the days and weeks after the journey, patients receive talk therapy to help them integrate the experience.

HOW DOES IT WORK?
A crucial factor in the psilocybin treatment’s effectiveness is whether the patient experiences a transcendent, often called “mystical,” experience during the session, Dr. Heinzerling says. “People will tell you that they saw the meaning of life, that they felt one with God or the universe, that their ego had dissolved,” he says. This experience can help patients have extraordinary insights into themselves and their behavior. “Traditional pharmaceuticals are useful in helping patients with depression or anxiety disorders feel better and those with substance abuse problems experience less cravings, but patients often relapse because underlying issues have not been addressed,” says Dr. Heinzerling. “And psychedelics like psilocybin can be a tool for a patient who wants to change and understand themselves better, even when it’s a hard process.” According to Daniel F. Kelly, MD, a neurosurgeon and PNI director, psilocybin mimics serotonin, a brain neurotransmitter. By stimulating serotonin receptors called 5-HT2A receptors throughout the cerebral cortex, life-altering and behavior-altering insights can be achieved. “Based on several landmark studies from major research institutions—including Imperial College of London, Johns Hopkins and University of Zurich—the working theory is that psilocybin affects the brain’s default mode network which is a large-scale network located predominantly in the frontal and parietal lobes of the brain and can be considered a neural construct for one’s ego,” he says. The default mode network seems to be where people get stuck ruminating about the past, worrying about the future, focusing on addictions and generating negativity. Psilocybin seems to unlock or dampen down the default mode network allowing much greater connectivity between brain regions that don’t normally communicate. While the exact mechanism of this brain reset is still not clearly understood, the result for many patients is truly life-changing, he says. “A remarkable aspect of psilocybin and similar compounds is that their impact is transdiagnostic, meaning they appear to be effective for not only depression and anxiety, but also possibly addiction and post-traumatic stress disorder,” Dr. Kelly says. A study published last year in the prestigious scientific journal Cell pointed to the effects of the substance on the 5-Hydroxytryptamine 2A (5-HT2A) receptor in the brain as a possible mechanism of action. Moreover, several landmark studies from major research institutions have brought research on psilocybin into the mainstream. Some of the studies include detailed brain imaging showing the physiological impact of the substance, he says.
HELP WITH ADDICTION
One of the most needed areas of mental health distress is for addiction including alcohol, nicotine and opioids. Psilocybin-assisted therapy has shown promise in several early clinical trials for these disorders. A recent study conducted by the NYU Grossman School of Medicine and presented at the American Psychiatric Association 2019 annual meeting found that one or two psilocybin sessions significantly reduced alcohol cravings. The TRIP program’s clinical trial for alcohol use disorder will investigate whether the number of subjects who have this epiphany-like experience, which is key to its success, can increase by changing the session’s setting. According to Dr. Heinzerling, patients in the TRIP alcohol use disorder study will be given 25 milligrams of a pharmaceutical, synthetic version of psilocybin that is identical to that in the genus Psilocybe mushroom. At the beginning of the session, half the patients have the standard setting, which is putting on eye shades and listening to music, which helps them focus internally. The other half will view a 40-minute nature-themed film with music created by award-winning filmmaker Louie Schwartzberg who produced the 2019 film Fantastic Fungi. “Researchers at the Imperial College in London have noted that reconnecting with nature can be therapeutic for people who have depression, anxiety or alcohol use disorder,” says Dr. Heinzerling. “We wanted to see if by including Schwartzberg’s Visual Healing films, we can increase that connection to nature to help people cut back or stop their alcohol use.” Thus far, five of 20 patients have already been enrolled in the study. Interest is also growing regarding psilocybin for helping with nicotine addiction. One small study from Johns Hopkins University found 70% of study participants who smoked had stopped smoking six months after a single psilocybin-assisted therapy session with preparation and integration sessions on either side of the psilocybin journey.
EMOTIONAL HEALING AND LONG-TERM RELIEF
Dr. Kelly says that TRIP is hoping to launch another psilocybin clinical trial for people with “complicated grief,” to be conducted in collaboration with Françoise Bourzat, a somatic psychologist and experienced guide, and Dr. Chris Adrian, a palliative care expert. “That trial looks to enroll 40 patients who lost a loved one during the COVID-19 pandemic and are suffering from prolonged grief of six months or more,” says Dr. Kelly. The need for more effective therapies to help people consumed by prolonged grief is all too apparent in the COVID-19 pandemic, when funerals and memorial services have been long postponed, says Dr. Heinzerling. “So many people who have lost loved ones to COVID-19 are suffering because they had to put their grief on hold.” TRIP is also planning research on the use of psilocybin to help terminally ill cancer patients who are experiencing anxiety, depression and other forms of spiritual distress, says Shanthi Gowrinathan, MD, director of psycho-oncology and cancer support services at the Saint John’s Cancer Institute and director of psycho-oncology at PNI. Research conducted at the NYU Grossman School of Medicine and published in the Journal of Psychopharmacology showed that one dose of psilocybin in combination with psychotherapy can provide cancer patients with long-term relief of emotional distress. “Psilocybin is markedly tailored for cancer patients because it’s relatively medically benign,” Dr. Gowrinathan says. “It’s fairly well tolerated and doesn’t have the side effects and issues that may make it hard to use for someone with cancer. ” Philanthropy helps support the meticulous biological and early clinical research that will help answer key questions about genus Psilocybe mushrooms, Dr. Heinzerling says. “We are grateful for the seed money we’ve received from the Annenberg Foundation and other private donors,” he says. Such research has the potential to pave the way toward much-needed, larger clinical trials. Therapies based on genus Psilocybe mushrooms may fill a void in psychiatry, says Dr. Gowrinathan, noting that one of her cancer patients who died recently had suffered severe emotional distress in her final months. “I wasn’t able to help her using traditional psychotropic medications,” Dr. Gowrinathan says. “I would have loved to have something else to offer her. I can’t put enough value on the ability to give someone peace of mind at the end of life. Nothing would be more rewarding than that.”
